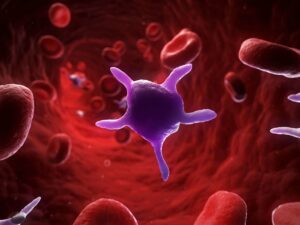
Platelet disorders encompass a range of conditions affecting the platelets’ function or quantity in the blood, leading to issues with blood clotting. Platelets, or thrombocytes, are small cell fragments in the blood crucial for forming clots to stop bleeding. Platelet count or function abnormalities can result in excessive bleeding or unwanted clotting. Understanding and managing these disorders is essential for maintaining overall health, particularly for those seeking care in a hospital in Kenya where advanced medical treatments are available.
Types of Platelet Disorders
- Thrombocytopenia
-
-
- Definition: A condition characterised by a low platelet count.
- Causes: This can be due to decreased production (e.g., bone marrow disorders, leukaemia), increased destruction (e.g., autoimmune diseases, certain medications), or increased sequestration in the spleen.
- Symptoms: Easy or excessive bruising, prolonged bleeding from cuts, spontaneous bleeding from gums or nose, heavy menstrual flows, and petechiae (small red spots on the skin).
-
- Thrombocytosis
-
-
- Definition: A condition where there is an abnormally high platelet count.
- Causes: Primary thrombocytosis (essential thrombocythemia) is due to bone marrow disorders, while secondary thrombocytosis can result from infections, inflammation, cancer, or splenectomy.
- Symptoms May include headaches, dizziness, chest pain, weakness, fainting, or, in severe cases, blood clots leading to stroke or heart attack.
-
- Platelet Function Disorders
-
- Definition: Conditions where platelets are present in normal quantities but do not function correctly.
- Causes: Genetic disorders (e.g., Glanzmann thrombasthenia, Bernard-Soulier syndrome), acquired conditions (e.g., use of certain drugs like aspirin), or secondary to other diseases.
- Symptoms: Similar to thrombocytopenia, including prolonged bleeding times, frequent nosebleeds, excessive bleeding after surgery or injury, and heavy menstrual bleeding.
Diagnosis of Platelet Disorders
Diagnosing platelet disorders involves several steps:
- Medical History and Physical Examination: Evaluating symptoms, medical history, and family history of bleeding disorders.
- Complete Blood Count (CBC): Measures the number of platelets in the blood.
- Peripheral Blood Smear: Examines the appearance of platelets under a microscope.
- Bone Marrow Aspiration and Biopsy: Assesses bone marrow function and platelet production.
- Platelet Function Tests: Evaluate how well the platelets work in clotting.
- Genetic Testing: Identifies inherited platelet function disorders.
Management of Platelet Disorders
The management strategies for platelet disorders vary depending on the type and severity of the condition:
- Management of Thrombocytopenia
-
-
- Treating Underlying Causes: Addressing the root cause, such as discontinuing offending medications, treating infections, or managing autoimmune diseases.
- Medications: In autoimmune cases, corticosteroids or immunoglobulins may be used to suppress the immune system. Thrombopoietin receptor agonists can stimulate platelet production.
- Platelet Transfusions: Used in severe cases to temporarily increase platelet counts.
- Surgery: Splenectomy (removal of the spleen) may be considered in chronic cases where the spleen is destroying platelets.
-
- Management of Thrombocytosis
-
-
- Observation: Mild cases may only require monitoring.
- Medications: Low-dose aspirin to reduce clotting risk; hydroxyurea or anagrelide lowers platelet counts in essential thrombocythemia.
- Treating Underlying Conditions: Addressing secondary causes such as infections or inflammation.
-
- Management of Platelet Function Disorders
-
- Avoidance of Medications: Avoid drugs that impair platelet function, such as NSAIDs.
- Desmopressin (DDAVP): Used to enhance platelet function in some disorders.
- Antifibrinolytic Agents: Medications that prevent the breakdown of clots, such as tranexamic acid.
- Platelet Transfusions: For severe bleeding episodes.
- Gene Therapy: Emerging as a potential treatment for genetic platelet function disorders.
Living with Platelet Disorders
Patients with platelet disorders can lead healthy lives with appropriate management and lifestyle modifications:
- Regular Monitoring: Regular check-ups with a healthcare provider to monitor platelet counts and function.
- Injury Prevention: Avoid activities that increase the risk of bleeding or bruising.
- Medication Management: Using medications as prescribed and avoiding those that can worsen the condition.
- Healthy Lifestyle: Maintaining a balanced diet, regular exercise, and avoiding smoking and excessive alcohol consumption.
Conclusion
Platelet disorders encompass a variety of conditions affecting the number and function of platelets, leading to significant bleeding or clotting issues. Proper diagnosis and management are essential to mitigate risks and improve quality of life. For individuals in Kenya, accessing care at a specialised hospital can provide the necessary treatments and support to manage these conditions effectively. With ongoing medical advancements and a commitment to patient care, hospitals in Kenya are well-equipped to handle the complexities of platelet disorders.